Illustration by Jim Cooke, from http://jezebel.com/a-former-abortion-doula-explains-why-an-iud-might-be-ri-1788962651
I wish I had gotten my IUD sooner. I’d been on the pill for eight years before I had one inserted, and didn’t know much about them until my best friend in college got one during our junior year. She went by herself, came home alone with a shrug: “It was easy. And totally free.” She had gone to Planned Parenthood, where they coached her through the process from start to finish without charging her a dime.
Three years later, I took the plunge. I did my research and went in for the initial consultation at Planned Parenthood (my only health care provider, at this point) which, because I was under their poverty guidelines and didn’t have insurance to cover it, didn’t cost anything. I asked a million questions and, with the help of my doctor, decided to get the Skyla. A few weeks, a couple Advil, and some mild uterine pain later, I had my new armor in place.
Getting an IUD has made my life remarkably easier and given me the security of knowing that I won’t get pregnant for the three years I’ll have it. They aren’t for everyone, but if you’re anything like me, you’ll love it.
What does an IUD do?
As you might have learned from JDP’s Birth Control 101 blog post, an IUD (intrauterine device) is a t-shaped device placed in the uterus that prevents pregnancy by disrupting sperm and preventing it from fertilizing an egg. Depending on the IUD, they can last anywhere from 3-12 years.
There are five different FDA approved IUDs in the US – four hormonal ones and one non-hormonal. The non-hormonal IUD (ParaGard) is wrapped in copper, which deters sperm and blocks it from getting to the egg. Hormonal IUDs (Mirena, Skyla, Liletta and Kyleena) prevent pregnancy by 1) thickening the cervix’s mucus, which blocks and traps the sperm and 2) stopping ovulation (during which eggs leave your ovaries). No matter what kind of IUD you get, they’re not permanent – as soon as you’re ready to get pregnant, you can have your IUD taken out, and you’ll be able to get pregnant within a month of removal.
How does an IUD get in there?
To insert an IUD, your care provider will check your vagina, cervix, and uterus, and should test you for STDs. When you’re ready to have it inserted, the doctor will use a tool called a speculum to open your vagina and cervix, then use an inserter to place the IUD into your uterus. Typically, this will take about five minutes, but insertion varies for everyone. There’s no way to predict how your body might react to getting an IUD inserted – some feel little to no pain during insertion and it goes in easily, but for others, it can be incredibly painful or difficult. To make sure you’re prepared, talk things over with your doctor, consult any friends you might know who have one, and read up on some of the guidelines later in the article. Easy peasy!
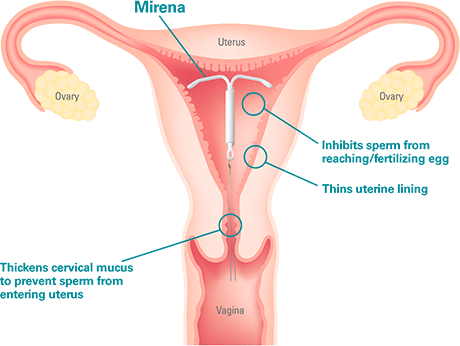
Diagram from www.mirena-us.com
Is the IUD right for you?
Though IUDs work well for most women, there’s a small margin of women who shouldn’t get an IUD. Planned Parenthood has some great information on who should not get an IUD. But the best way to know if an IUD is right for you is to chat with a provider directly. Set up an appointment with a provider and see what they suggest for you. You can also take this Bedsider quiz beforehand. Planned Parenthood also has a great step-by-step process for narrowing your method down.
Which IUD is the right fit?
If you do decide to get an IUD, take some time to research or talk to your provider about the different kinds of IUDs available. When you decide on one, make sure your prefered clinic has that brand in stock before booking your appointment.
There are four kinds of hormonal IUDs:
The Mirena works up to six years, Kyleena up to five, and Skyla and Liletta up to three. All of them use a hormone called progestin, which is found in all other forms of birth control. Liletta and Mirena use the highest dose of hormone out of the four, Kyleena a little less, and Skyla the least of all. All of them make periods lighter for most people, and many stop getting their periods altogether.
As for non-hormonal, there’s just the one:
The ParaGard is currently the only non-hormonal IUD in the US, and can last up to twelve years. ParaGard also works as emergency contraception, and can prevent pregnancy up to five days after unprotected sex. However, ParaGard typically makes periods heavier and longer, with sometimes more severe cramping.
For more information on all five IUDs, check out Bedsider’s awesome guide, or their step-by-step guide to preparing for an IUD.
Does my IUD protect me from sexually-transmitted diseases?
No. Make sure you know your partner’s sexual history, and wear a condom. IUDs give no protection against any STIs.
So how can I get one??
If you have insurance, an IUD will probably be covered! To be safe, though, talk to your insurance company and your doctor to figure out what parts, if any, of the process they’ll cover: do they cover the device itself? The insertion visit? The informative pre-insertion visit? What about follow up visits? Make sure you know what your health insurance will provide.
If you don’t have health insurance, you may be eligible for free or low-cost IUD services. You can call your local Title X clinic to set up an appointment to find out your eligibility. You can also consent to an IUD on your own, without needing a parent, at any Title X clinic. Bedsider also has a great tool for finding out where else you might qualify for a free or low-cost IUD.
Once you’ve covered all your bases with coverage, it’s time to find a clinic and set up your appointment! Make sure you know which clinics are available to you, and which ones offer IUD insertion services. Ask your provider what you should bring with you – they’ll probably ask for your health insurance card, and possibly some form of ID.
Party time
You did it! You booked an appointment. Now it’s time for your IUD to get inserted. Here are a few things to do before your appointment:
Take an aspirin or an advil. As mentioned before, the procedure can be painful. While the pain varies for everyone, it often feels like an intense, longer version of a menstrual cramp. The pain is a result of your doctor opening your cervix to insert the IUD, which is why many experts suggest scheduling your insertion during your period, when your cervix is naturally a little open. You can also talk to your doctor about getting a prescription for misoprostol, a drug that causes your cervix to dilate, before the insertion.
Secure a ride. Depending on your reaction to the insertion, you may not be up for driving immediately afterwards. While I drove myself home, I was grateful to have my best friend present, who could have driven if needed.
Wear loose clothing. After the insertion, you might not take kindly to a too-tight waistband. As an extra bonus, wearing a dress makes undressing for the insertion quick and easy.
Bring your own panty-liners. My clinic had some pads handy, so I got lucky. But you’ll be happy to have these just in case, because you’ll likely have some light bleeding after the insertion. Or, for a really pro tip and extra comfort: order some spotting-absorbing underwear, if you can swing it.
Bring your ID and health insurance card. As mentioned before, your clinic will probably ask you to bring these along. If you don’t have an ID or health insurance, call your clinic to see what your options might be.
Bring a book or magazine for distraction. Of course, your provider might have some handy, but I found myself waiting longer than I anticipated for my doctor, which amped up my nerves. I was ill-prepared, so I turned to Instagram, which was a vital distraction for me as I waited it out.
Book a check-up visit. Your provider should remind you to do this anyways, but make sure you book a check-up within a month or so to make sure your IUD is still in the right position. You can also ask your doctor to show you how to check for the strings yourself.
Take it easy. Your doctor might prescribe pain meds, but make sure to have some ibuprofen on hand to ease your cramps. You’ll probably want to take it easy for the rest of the day, since you’ll likely have some discomfort after the insertion. For my roommate and I, this was a good excuse for a spa day at home – tea and hot pads help, in addition to the Advil. Celebrate! You just got some fancy new armor. Make some brownies, put Netflix on, and rejoice!
Check in with your body. After your IUD has been inserted, make sure you’re monitoring your body for any abnormal pain or reactions. Moderate to heavy cramping is normal, but ongoing pain or abnormal discharge may be signs of infection, so keep an eye out and call your doctor with any questions.
You should also keep track of your mood and mental state. For some, the IUD’s hormones can be disruptive and cause emotional imbalance, so make sure you’re listening to your body. While your doctor can offer advice, you ultimately know your body best – if it doesn’t feel right, it’s not for you. You should always feel comfortable advocating for yourself, even with an expert like a doctor.